Maternal Health Initiative - 1st Year in Review
The Maternal Health Initiative (MHI) works in northern Ghana delivering a light-touch programme of training integrating contraceptive counselling into routine care to increase informed choice and uptake of family planning methods. We deliver this work in partnership with two local NGOs and the Ghana Health Service, launching through the 2022 Charity Entrepreneurship Incubation Programme.
Summary
In our first year, we…
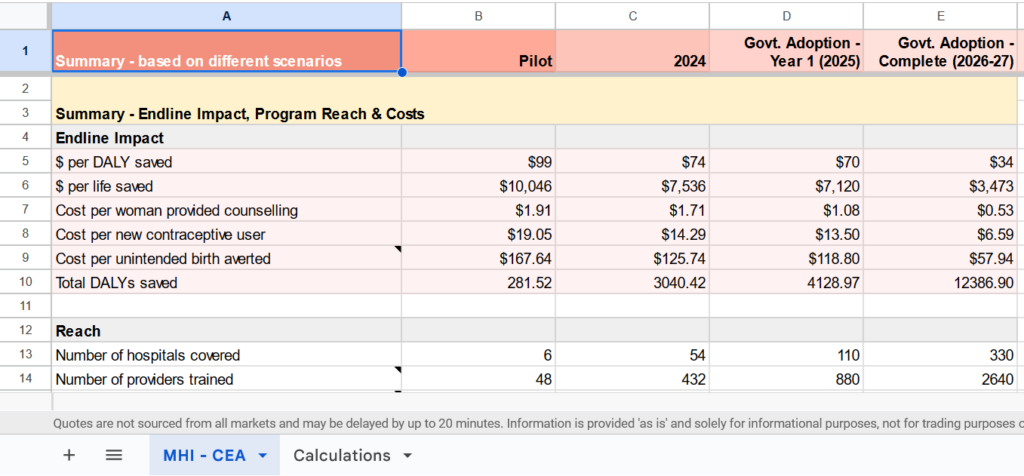
- Developed and tested two evidence-based models of care with an estimated cost-effectiveness of $100/DALY on health effects alone, competitive with GiveWell’s top charities
- Trained providers at 18 facilities across 2 regions of Ghana, reaching an estimated 40,000 women over the next year
- Conducted in-depth on-the-ground research, surveying 836 women and 148 providers & facility directors
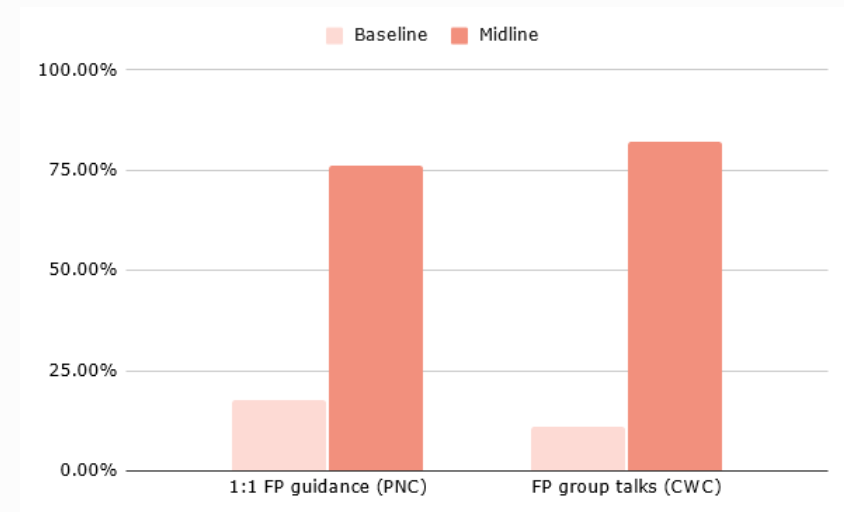
- Successfully increased the frequency of 1:1 family planning counselling by 4.3x at postnatal care and group family planning messaging by 8x at immunisation sessions, with results for shifts in contraceptive uptake due in December 2023.
We’re currently awaiting our full results from our pilot. With strong results, we plan to scale our work through 2024 in partnership with the Ghana Health Service as we build towards government adoption of our model of care.
Who are MHI?
Maternal Health Initiative is an early-stage global health charity with a focus on healthcare worker training and access to family planning. MHI was born out of research conducted by Charity Entrepreneurship identifying postpartum (post-birth) family planning as among the most cost-effective and evidence-based approaches for improving global health.
Our team now includes Sofia Martinez Galvez as our Program Officer, Sulemana Hikimatu Tibangtaba as our Training Facilitator, and Enoch Weyori and Racheal Antwi as Project Officers through our local implementing partners, Norsaac and Savana Signatures.
What we do
We train midwives and nurses in the integration of two new models of family planning counselling developed by MHI into the standard check-ups mothers and their children receive in the months after giving birth.
In doing so, our work increases postpartum contraceptive uptake and decreases the frequency of short-spaced births. Pregnancies that occur less than two years apart are associated with a 32% higher rate of maternal mortality and 18% higher rate of infant mortality (Conde-Agudelo 2007; Kozuki 2013). Despite these risks, contraceptive use in Ghana drops by two-thirds in the early postpartum period.

Integrating high-quality counselling into routine care addresses multiple barriers to contraceptive uptake. First, mothers do not need to travel to a facility specifically for family planning. This means that they can receive confidential information and that they are spared the costs – both in time and money – of a separate visit.
Second, many women express significant concerns around side effects and health consequences from family planning. High-quality counselling ensures women receive counselling on multiple methods – helping to find a method that avoids the side effects they may be concerned about – while addressing myths and misconceptions that can drive opposition to the use of methods.
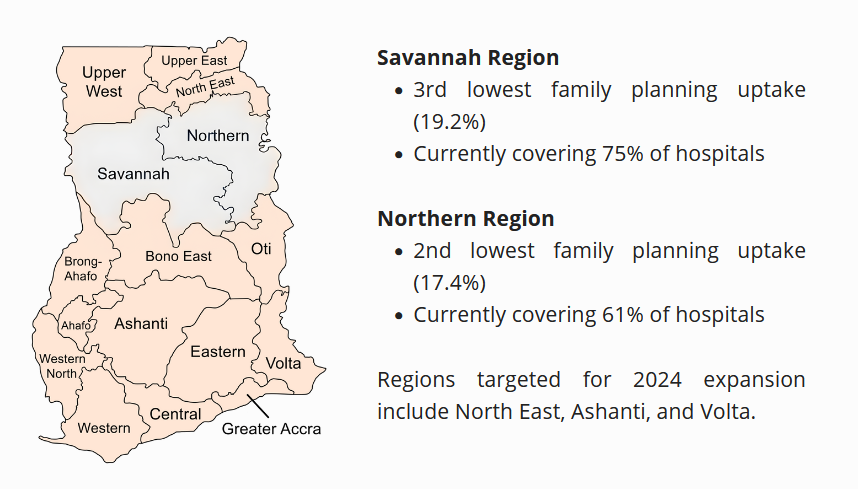
Why Ghana?
One of our first decisions was choosing which country to operate in. We conducted field visits to Sierra Leone and Ghana in January 2023 after an extensive process of research, data evaluation, and expert engagement that identified these as the best choices out of 44 countries considered.
Statistically, Ghana has a high unmet need for family planning and significant maternal and infant mortality, while having one of the highest levels of facility delivery and most robust governance structures in sub-Saharan Africa. Government integration provides a route to potentially transformative cost-effectiveness at scale, making the last two factors – level of facility delivery and governance quality – particularly crucial to our work.
Models of care
Our work is built around two models of care (program arms), targeting different points in the continuum of care after delivery. Each program is built directly off an RCT of a similar model (Asah-Opoku et al., 2023; Dulli et al., 2016), with a large body of evidence demonstrating the impact of postpartum family planning more broadly.
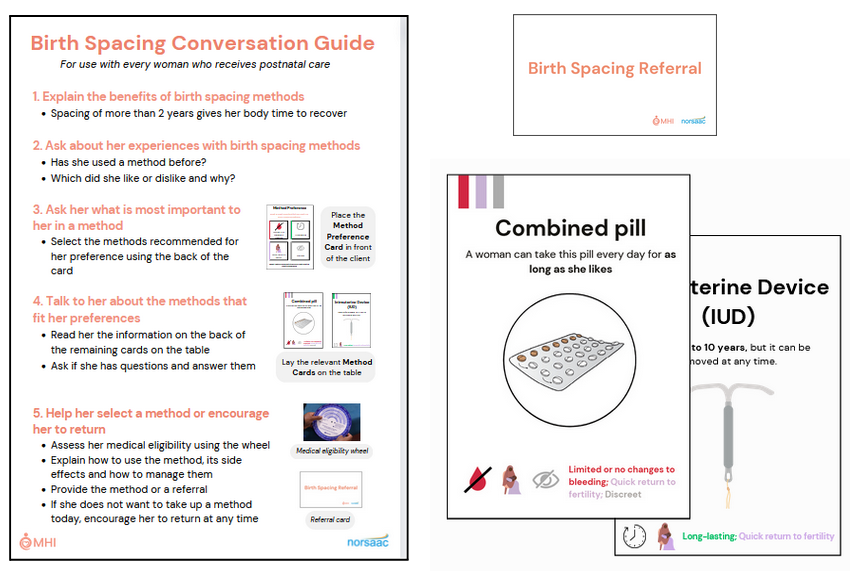
The postnatal care (PNC) arm integrates 10-15 minute family planning counselling into existing individual one-on-one appointments that take place 48 hours, 2 weeks, and 6 weeks post-birth. We developed a conversation guide and method cards to facilitate sessions and emphasise the delivery of client-centred care.
The child welfare clinic (CWC) arm targets the monthly sessions mothers attend from six weeks onwards with a primary focus on their child’s health and wellbeing. Our programming adds a group talk on family planning as well as brief, 1:1 counselling on family planning during vaccination into these sessions. We developed a flipchart for the group talk, as well as a card for very brief discussion during the 1:1 engagement.
For both of our program arms, we have carefully designed materials that are specifically tailored to the point of care and needs of the women we serve. Hospitals can be understaffed with providers overstretched, making it crucial to design improvements to care that are feasible and easy for providers to use. We have received consistently positive feedback from providers on the practicality of our tools.
Program Delivery
This year, MHI ran three major projects covering 18 facilities across two regions of Ghana. In total, we estimate around 40,000 women will receive MHI’s model of counselling through these projects.
Proof of Concept
In April 2023, we ran our first two training sessions at the conclusion of an extensive process of qualitative research in which we interviewed 151 clients and providers.
One key aim was to understand the feasibility of delivering single-day training sessions. Most other family planning training interventions we researched involved multi-day or even multi-week training sessions. One-day training placed significant time constraints on our program delivery with obvious and significant cost-saving benefits.
Data from two of the six facilities indicated a 15% increase in contraceptive uptake in the three months after the training sessions. This gave us confidence in the feasibility of our training delivery, while feedback from the providers and our partners helped us refine our programming models.


Mini-pilot
We launched a ‘mini-pilot’ in July 2023, training 45 providers from hospitals across two regions. Ahead of these training sessions, we shifted to the two models of care described above, more specifically tailoring the training and materials we provide to the points of care at which they will be used.
These training sessions focused on refining the materials and ensuring consistent implementation of the models of care. One-month follow-up data from this project indicates a 4.3x increase in 1:1 counselling at postnatal care and an 8x increase in group counselling at immunisation sessions.
Mini-pilot
These trainings took place in October 2023 after ethical approval from the Navrongo Health Research Centre. We trained 50 providers from six hospitals in the Northern Region. These hospitals receive an estimated 20,000 clients annually.
We are currently conducting a six-week follow-up at these facilities to measure contraceptive uptake as a result of the intervention, through both in-person and phone surveying. These results will form the basis of MHI’s 2024 programming decisions and further engagement with the Ghana Health Service on next steps towards national programme adoption.

Our Impact
Estimating the impact of behaviour change interventions is tricky, especially for earlier-stage programs for which long-run data comparisons and evaluations are not possible. We estimate that our pilot programme will avert a disability-adjusted life year (DALY) for just under $100, competitive with the cost-effectiveness of GiveWell top charities such as AMF. If we are successful in achieving government adoption of the program, we estimate the cost per DALY would drop to just $34 while reaching around 800,000 mothers annually.
Beyond this, we firmly believe in the value of the non-health benefits of family planning access. Control over whether and when to have children is a fundamental marker of personal autonomy. There are robust arguments in favour of a much broader view of doing good, with prioritisation on the basis of subjective wellbeing or the capabilities approach providing two examples.
Discussing the merits of these is far beyond the scope of this post, but we believe the fundamental influence child-bearing has on people’s lives makes providing high-quality counselling for less than $2 per person highly valuable beyond its direct health implications.
Our Plans (for 2024 and beyond)
As mentioned above, we will have the results of our pilot program in December 2023, including its impact on contraceptive uptake (the rate of contraceptive use). We have mapped out three scenarios for our 2024 work based on the success of the pilot and on the level of funding we raise in the coming months.
If the results of our pilot are strong, we plan to design a final large-scale evaluation of the most promising programming model (PNC or CWC) in partnership with the Ghana Health Service. This would be explicitly designed to model a fully-integrated model of the program that the government would be open to adopting as part of the Ghana Health Service’s systems and policy should it prove successful.
With weaker results, we will focus on a smaller test of a redesigned model of care, dedicating more resources to testing potentially transformative changes to the delivery of our work, such as a Whatsapp-driven model of training delivery, that could make direct program delivery exceptionally cost-effective in its own right.
How to support us
Donate
If you would like to support our work, you can donate directly through our website. Donations are fully tax-deductible for US tax residents. For larger donations, we’d love to speak to you personally to answer any questions you may have about our work – please reach out through our contact page.
Recommend to a friend
If you know someone who might be interested in supporting our work, we’d love you to recommend us to them – by sharing this article, by linking to our website, or encouraging them to join our newsletter.
Follow our work
If you’d like to stay in touch with our work, we’d love to keep you informed. Follow us on LinkedIn, Facebook, or subscribe to our newsletter.
